Blog
Travel Vaccine Blog

By Munir Dharamshi
•
25 Jan, 2024
UNDERSTANDING CHOLESTEROL TO BETTER CONTROL IT In Canada, cardiovascular disease is the second leading cause of death after cancer. High cholesterol is one of the risk factors for cardiovascular events that can be controlled. Therefore, it is important to understand the role of cholesterol and what can be done to reduce high blood cholesterol levels. WHAT IS CHOLESTEROL? Cholesterol is a fatty substance produced by the liver. It plays several key roles in the body, including the production of hormones (e.g., estrogen, testosterone), vitamin D, and bile, an important substance for fat digestion and nutrient absorption. In order for cholesterol to circulate in the blood, it must attach itself to transport proteins to form what is known as a lipoprotein. The two main lipoproteins are: low-density lipoprotein (LDL) cholesterol and high-density lipoprotein (HDL) cholesterol. LDL-cholesterol is transported from the liver to the cells and is sometimes called "bad” cholesterol. HDL-cholesterol is sometimes called "good" cholesterol because it helps in the removal of excess cholesterol by carrying it out of the cells. WHAT ARE THE CONSEQUENCES OF EXCESS CHOLESTEROL IN THE BLOOD? When too much LDL cholesterol is present in the blood, it can settle on the walls of blood vessels and form deposits called plaque. Over time, if the level of LDL-cholesterol in the blood remains too high, this plaque will continue to grow, gradually reducing the space available for blood to pass through. It is possible to have plaque in more than one artery at a time. Plaque can also break into pieces and form clots that can completely block the passage of blood. If the blockage occurs in the heart, it causes a heart attack. If it occurs in the brain, it causes a stroke. WHY DO SOME PEOPLE HAVE TOO MUCH LDL-CHOLESTEROL? Several factors increase the risk of high LDL-cholesterol, such as: Poor diet, especially high in trans fats and/or saturated fats Sedentary lifestyle Being overweight Chronic stress Smoking Aging Most LDL-cholesterol (about 80%) is produced by the liver, regardless of our lifestyle. In some families, high cholesterol levels are caused by an inherited disease. woman watching tv WHAT ARE THE SYMPTOMS OF HIGH CHOLESTEROL LEVELS IN THE BLOOD? LDL-cholesterol itself does not cause any symptoms. It is usually discovered to be too high when blood tests are done as part of a check-up, or when the person has a cardiovascular event such as a heart attack or stroke. WHAT CAN BE DONE TO LOWER CHOLESTEROL LEVELS? Lifestyle modifications are essential for managing high cholesterol. Here are some recommendations to improve your lifestyle. Eat a healthy diet Engage in regular physical activity Achieve and maintain a healthy weight Manage stress Stop smoking 1. Eat a healthy diet The typical North American diet is often high in animal products (e.g., red meat, processed meats, high-fat dairy products) and processed foods that may contain cholesterol, but most often saturated or trans fats. Because these types of fats increase the liver's production of LDL-cholesterol, you should limit the amount you eat. Foods that are high in cholesterol but low in saturated fat (such as egg yolks, some seafood, and organ meats) can be eaten in moderation. To make lasting improvements to your diet, make incremental changes. Start by removing processed foods from your diet. Try to cook your own meals to ensure they contain healthy ingredients, such as Plenty of fruits and vegetables High-fiber foods (e.g., barley, oats, quinoa) Plant-based proteins, such as beans, lentils, tofu, or nuts Small amounts of lean meats If you need help improving your diet, talk to a registered dietitian. 2. Engage in regular physical activity Studies have shown that people who are physically active have higher levels of HDL-cholesterol, the "good" cholesterol, than sedentary people. Regular physical activity also improves both physical and mental health, and contributes to weight loss and stress reduction. You do not have to become a top-level athlete! It is recommended that you exercise on a regular basis, for at least 30 minutes a day and at least five times a week. Choose an activity that fits easily into your routine, such as walking. If you're having trouble getting motivated, join a friend, colleague, or club. If you have a chronic health condition, talk to your health care team to find out if there are any restrictions that you should be aware of. 3. Achieve and maintain a healthy weight Obesity is associated with higher levels of LDL-cholesterol and lower levels of HDL-cholesterol. Improving your diet and/or physical activity may help you lose weight. For medical treatment of obesity, you should consult a healthcare professional. 4. Manage stress Studies have shown that people who experience prolonged periods of stress have higher levels of LDL-cholesterol. Learn different techniques to reduce stress, such as meditation, mindfulness, breathing, or relaxation techniques. Try to identify the sources of chronic stress in your life and see if you can reduce or eliminate them. This often isn't easy and may require you to question certain priorities, but making these important changes will benefit your overall health and quality of life. 5. Stop smoking Smoking lowers HDL-cholesterol and increases the risk of cardiovascular disease. If you smoke, talk to your pharmacist. In most provinces, pharmacists can prescribe smoking cessation medication to help you quit for good. Do not hesitate to ask for advice. WHEN SHOULD PHARMACOLOGICAL TREATMENT BE CONSIDERED? If you are not at high risk for a cardiovascular event (such as a heart attack or stroke), you will usually start with lifestyle changes before considering drug treatment. If LDL-cholesterol levels are still too high after a few months of lifestyle changes, drug treatment may be prescribed. However, if your LDL-cholesterol is very high, or if you are at high risk for a cardiovascular event (for example, if you have had a heart attack or stroke, or if you have diabetes or chronic kidney disease), drug treatment should usually be started at the same time as lifestyle changes. Several medicines can lower LDL-cholesterol. Your healthcare provider will prescribe the one that is best for you. YOUR PHARMACIST, YOUR ALLY TO ACHIEVE YOUR GOALS If you have questions about cholesterol or cholesterol-lowering medicines, see your pharmacist. In addition to answering your questions, your pharmacist can help you make lifestyle changes and refer you to other professionals, such as a registered dietitian or kinesiologist, if needed. In some provinces, pharmacists may offer a service to help you achieve your cholesterol reduction goals. Check with the staff at your local pharmacy for more information.
By Munir Dharamshi
•
25 Jan, 2024
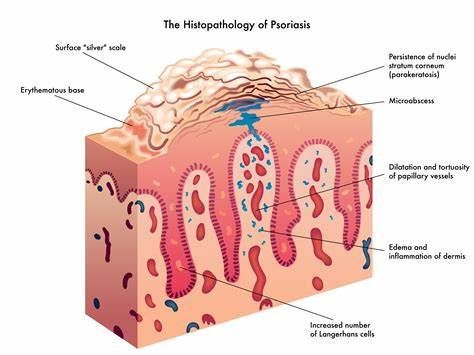
WHAT IS ECZEMA? Eczema is a general term that refers to a group of diseases characterized by an inflammation of the outer layer of the skin. The word “eczema” is widely used to refer to the atopic form of the condition (also known as atopic dermatitis), and is the term we use in this text. It is the most common type of eczema: 17% of Canadians will suffer from it at some point in their lives. Eczema is usually hereditary. This means that children whose parents have eczema are more likely to suffer from this skin disease, and also to develop asthma or hay fever. In most cases, eczema first appears in early childhood. With eczema, the barrier that protects the skin from external elements fails to play its protective role properly, allowing various irritants or allergens to penetrate the skin more easily. In addition, the immune systems of people with eczema overreact to these irritants and allergens, causing an inflammatory reaction. WHAT IS PSORIASIS? Psoriasis is not as common as eczema. It is estimated that 2% to 3% of Canadians suffer from it. Psoriasis is an auto-immune skin disease, which means the immune system mistakenly attacks the skin cells. The term “psoriasis is often used to refer to the plaque form of the disease, which primarily affect adults. It is the most frequent kind (90% of cases). When psoriasis occurs in children, it is generally in the form of guttate psoriasis (teardrop-shaped spots). WHAT DO ECZEMA AND PSORIASIS LESIONS LOOK LIKE? The lesions caused by eczema and psoriasis have certain similarities, but also several distinctive characteristics that enable your health professional, for example, a family doctor or dermatologist, to make a diagnosis. Characteristics Atopic Eczema Plaque Psoriasis Appearance of skin lesions Red, dry, swollen areas of skin combined with often intense itchiness Sometimes the lesions can weep, become scaly, or form scabs. Dry or red skin plaques with clearly defined edges. Plaques are covered with silvery-white scales that come off in flakes. Lesions are sometimes painful or itchy. Location of lesions Anywhere on the body, but typically in the crook of the knees and elbows, or on the face, neck, or hands Anywhere on the body, but typically on the elbows, knees, scalp, chest, or lower back People with psoriasis can develop a complication known as psoriatic arthritis, which causes swelling and pain in the joints. People with eczema tend to scratch a lot because of the itchiness, which can lead to skin infections and skin thickening (lichenification). WHAT TRIGGERS ECZEMA OR PSORIASIS SYMPTOMS? Eczema and psoriasis lesions often appear in a cyclical fashion, i.e., they can flare up suddenly then disappear for a while (remission), then reappear when something triggers them. Eczema flare-ups can be triggered by exposure to an allergen or irritating substance such as a chemical product, or to a rough-textured fabric, such as a wool sweater, that can irritate the skin. Environmental factors can also trigger symptoms, including extreme temperatures or very dry air. An eczema flare-up can also be triggered by a period of stress, an infection, or after eating certain foods. With psoriasis, flare-ups are often triggered by sunburn or an injury (even a minor one) to the skin, for example nicking yourself when shaving, or an insect bite, a scratch, a bruise, or a blister. Some medications can also bring about psoriasis or cause a flare-up. Certain other psoriasis triggers are similar to those that occur with eczema, including stress, an infection, or cold and dry weather. Psoriasis flare-ups are more common in people who suffer from obesity or who smoke. HOW IS ECZEMA TREATED? The treatment for eczema aims primarily to reduce inflammation and relieve symptoms. It should be adapted to the severity of the eczema, and may include the following: Daily use of an emollient cream to keep skin moisturized and prevent eczema flare-ups. It must be applied daily, during and between flare-ups. Application of a topical corticosteroid to reduce skin inflammation during eczema flare-ups. In very severe cases, injectable biologic drugs may be required. Antihistamines, especially at night, to relieve itching HOW IS PSORIASIS TREATED? The treatment for psoriasis also focuses on reducing inflammation and managing symptoms. It may include the following: Topical creams and ointments: Corticosteroid, retinoid, or vitamin D-based products may be prescribed to reduce inflammation and thick plaques. Light therapy: Light therapy, or UVB treatment, consists of exposing the skin to controlled doses of ultraviolet rays, to reduce inflammation. Systemic drugs: In the most severe cases, oral or injectable medications such as immunosuppressive drugs may be required, to modulate the immune system response. Biologic treatments: Biologic treatments are an option for patients with severe, chronic psoriasis. They target immune system–specific proteins responsible for inflammation. Identifying and avoiding triggers is also key to treating eczema and psoriasis. Reach out to your pharmacist for advice on which products to choose for your specific needs, for example a gentle soap or emollient cream. If you have questions about how to treat eczema or psoriasis, ask your pharmacist. They are there for you!

By Munir Dharamshi
•
18 Jan, 2024
With travel largely back to pre-pandemic levels, you may wonder what's safe. It mainly depends on whether you're up to date on your COVID-19 vaccinations. Here's what to know if you're taking a trip within the U.S. or abroad. Vaccinated Travel You're less likely to get seriously ill from COVID when you travel if you're up to date on your vaccine. That means getting the most recent version of the shot. Vaccines made by Pfizer, Moderna, and Novovax have all been updated to protect against the most widely circulating strains. If you're fully vaccinated but also have a weakened immune system because of a health condition or a certain medication, ask your doctor what travel precautions you should take. You don't have to wear a mask anymore on airplanes, buses, trains, cruise ships, or other types of public transportation, but sometimes it's still a good idea. The CDC recommends you wear one when you’re in areas where the rate of hospital admissions related to COVID is high. If you're at an increased risk for severe illness from COVID or live with someone at higher risk, talk to your doctor about wearing a mask at medium COVID hospitalization levels. To find out the COVID situation at your destination, you can check with local health departments or visit the CDC website. Their COVID Data Tracker tool can show you the level of COVID-related hospitalizations in a particular county. If you've been exposed to the virus, you’ll need to take certain steps whether or not you're traveling. You should wear a mask around others for 10 days and test for COVID at least 5 days after your exposure. Stay away from people who may be at higher risk for severe COVID. If you develop symptoms, get a test and stay home. Do I Need a COVID Booster? Studies show that COVID vaccine protection fades over time and that booster shots help. The CDC recommends that everyone get the most current version of the COVID shot. That's regardless of how many doses you've already had. Pfizer and Moderna vaccines are approved for adults and children as young as 6 months, while the Novovax vaccine is approved for everyone 12 and older. Most people just need one shot, although dosing schedules are different for children between 6 months and 4 years. Unvaccinated Travel It's riskier for you to travel if you haven't gotten the COVID vaccine or if you don't have its full protection yet. It takes about 2 weeks for the shot to boost your immune system. People who aren't vaccinated are more likely to catch the virus and spread it. Don't travel if you: Feel sick Have had a COVID test and are waiting on the results Got a recent positive test result Think you've been around someone with COVID If you're traveling without being fully vaccinated, you can take some steps to protect yourself and the people around you: Get a COVID test 1 to 3 days before you leave. Wear a mask on public transportation and in airports, stations, and other travel hubs. Keep your distance from people who aren't traveling with you. Wash your hands often or use a hand sanitizer. After you come back from your trip, you may want to consider staying home and getting a COVID test within 3 to 5 days. Vaccine Passport A vaccine passport is proof that you’ve tested negative for or been protected against certain infections. It can be digital, like a phone app, or physical, such as a small paper card. You can carry it with you and show it if required, like before you go into the office, board an airplane, or visit a restaurant, movie theater, or gym. When COVID vaccines first became available, the concept of a vaccine passport system was raised as a way to help boost economies while limiting the spread of the disease. Companies would be able to fully open for business to people who were vaccinated. It was a new play on an old idea. For years, people who’ve traveled to certain areas of the world have needed to show papers -- or a medical passport called a yellow card, created by the World Health Organization (WHO) -- to prove that they’ve gotten vaccines against diseases like yellow fever. But ultimately, it didn't happen. While most countries required proof of a COVID vaccination or a negative test to enter during the pandemic, it was temporary. Nearly all of those restrictions have been lifted. Does It Matter How I Travel? No matter how you go, being around people who don't live in your household raises your risk of getting and spreading COVID. But you can stay safe with some precautions while using different modes of transportation. Air travel. The CDC recommends that you check the level of COVID hospitalization at your destination before you go. If it's high, you may want to postpone your trip -- especially if you're at a higher risk for severe illness. If you're healthy, your risk of catching the virus on a plane is pretty low. The air on planes goes through a filter that catches most viruses and other germs. If you want to be extra safe, you can wear a high-filtration face mask when you’re in airports and on planes, and clean off your seat and tray table with a disinfectant wipe before you sit down. You're more likely to get infected if you sit close to someone who's sick. If someone near you is coughing or looks ill, ask the flight attendants to move you or that person to a seat at least 6 feet away. Cruise ships. The pandemic shut down the cruise industry for months. When sailings resumed, the CDC had rules for companies operating in U.S. waters about testing for passengers and crew, cleaning procedures, and other virus safety measures. Now there are guidelines for preventing the spread of COVID-19 and other respiratory viruses, which recommend: All crew and passengers over age 6 months have the latest vaccines Passengers get tested before they board Passengers reschedule their trip if they're sick Cruise lines test and isolate passengers who show symptoms Ships have handwashing or sanitizing stations available Passengers and crew consider wearing a mask in crowded or enclosed places. No matter which mode of transportation you take, carry a mask in case you find yourself in a crowded place. Avoid touching common surfaces as much as you can. Use hand sanitizer before and after travel, and wash your hands with soap and water when you get to your destination. International Travel Restrictions The restrictions and requirements that were in place throughout the pandemic have been lifted for the most part. But you should still check with the country you're traveling to, and the airline or cruise company you're using, about their specific rules. The CDC keeps a list of travel notices for places around the world at CDC.gov/travel. You can check whether you need to take special precautions against COVID or other diseases. The U.S. State Department also lists vaccine requirements for entry to global destinations at travel.state.gov. What if I Get COVID-19 When I Travel? Plan for how you’ll pay for health care before you leave. Check with your insurance provider to see if they’ll cover general or emergency medical expenses in the U.S. or abroad. If they don’t, consider buying additional short-term travel insurance. If you test positive for COVID-19 during your trip, you may need to stay longer at your destination while you isolate. You’ll want to consider the costs of extra lodging or last-minute travel changes. If you're traveling internationally, do some research ahead of time to find out whether the country has isolation or reporting policies and when you'll be cleared to travel. Up-to-date COVID vaccines can protect you from a serious illness. But talk to your doctor if you’re worried about getting sick when you travel. They’ll let you know if there’s more you can do to stay safe.

By Munir Dharamshi
•
18 Jan, 2024
It feels like everyone is getting sick right now. Hospitals are struggling with what the Canadian Medical Association called an “avalanche of patients,” and many of you have questions about what’s causing the illness and what to do about it. The Globe’s health reporter Carly Weeks joined The Decibel podcast to explain how this year’s respiratory virus season is shaping up, answering reader questions about COVID-19, RSV, the flu, and more. How would you describe this virus season that we’re having? We’re right in the thick of it in respiratory virus season, we see this every year. What’s really different is that for the past few years, it’s really been unusual. I don’t have to remind people that we’ve just been through a pandemic and according to who you ask, we’re kind of still going through it. That’s because COVID-19 is not yet at a predictable enough place to really say that it’s a seasonal virus, like the flu, and that can complicate things. There were a few really quiet years when a lot of people were at home, masking, and things were closed down because COVID-19 was top of mind, so flu numbers were down. Last year, we saw numbers come back in a huge way. This year, there are a lot of regions in the country that have had a really hard time, or are having a hard time currently. No matter where you look, there are pockets of the country that are really seeing a lot of sick patients coming in and the health care system is seriously under strain. But at the same time, the overall numbers themselves don’t look as though they’re beyond the scope of what you might see in a say, a very bad flu year. But the important context is that our health care system is already at or over capacity. So adding any sort of regular flu season on top of that, let alone a bad one is going to have a great impact. Where are we seeing cold, flu and RSV season the worst? If you look across the country, there are various regions that are seeing different things. A few weeks ago, I was speaking to officials and clinicians in Alberta and they were getting absolutely hammered by the flu. They were seeing lots of people getting admitted, including children. In Ontario, they were seeing higher numbers of RSV. This week, we’re hearing from B.C. health officials that they’re basically in a state of crisis because of flu numbers and other respiratory viruses going around. Quebec has seen really, really high numbers and a health care system that is barely functioning. As one region peaks and starts to decline, another region is seeing a huge increase. That’s just how virus is spread, right? It’s not going to be all at once. This is likely a warning to the rest of the country. If you haven’t seen really bad numbers, or if you’re in a province where cases aren’t yet at their peak, they likely will start to peak. What’s the difference between RSV, COVID-19 and flu? And how would you know if you have one versus the other? They’re all common respiratory viruses that get spread around. The virus likely enters through the upper respiratory tract when someone coughs or sneezes nearby. The difference between them can be a bit hard to distinguish. You can typically tell if it’s the flu based on how severely impacted you are, as it’s more severe than the common cold. The flu symptoms are more extreme – you have a high fever, you’re totally aching, lots of fatigue. RSV is another very common virus that essentially everyone gets by the time they’re age two, and then you can get reinfected with it. For most people it basically is a common cold: coughing, sneezing. But it can be very serious for young children, particularly those two and under, especially six months and younger or older adults. COVID-19 is a bit of a different beast, it’s continuously shifting, and it’s not yet very predictable. The symptoms can look like common cold in some people, there’s still things like the loss of sense of taste and smell. What we’re hearing from a lot of people now is that the symptoms may not look the same person to person, it’s a very tricky thing to tell. Unless you’re in an emergency room and a doctor’s ordering a panel of tests, you may not know what you have. Are we seeing higher numbers of illness now that COVID-19 is in the mix? It’s hard to say without a really deep, well researched study if we are seeing more people getting sick more often. I think it is fair to say that we have been through a very unusual period, and we’re not necessarily out of it yet. So when you do have an extra virus added into the mix, it has certainly had a big impact. According to the most recent federal data, there are nearly 5,000 patients with COVID-19, who are currently in hospital right now across the country. So having that extra virus, on top of our other seasonal viruses, is certainly adding to the challenge. Do we have reduced immunity because we didn’t really get sick during the pandemic? There was this idea going around, that has largely been debunked, that because we weren’t sick for so long we’re now more at risk from illness. Really what’s happened is that people who didn’t necessarily get impacted by illness for a couple of years just started getting sick again when we started mixing again, and illnesses started going around. Are illnesses lasting longer right now? Anecdotally, a lot of people are getting sick, and a lot of people are getting sick with numerous things. Whether or not people are getting sick for longer periods, is a bigger question. What experts would say is that because there are so many viruses going around and a lot of people who are at risk – maybe they haven’t been vaccinated, maybe they’re in close contact with people they haven’t seen in some time – they’re likely getting a couple of different things. We know that viruses like COVID-19 can lead to longer lasting symptoms in some people, feeling unwell for weeks on end. I think it’s fair to say that people are going to be experiencing more illness in the coming weeks before things start to settle down. Are we seeing data about flu numbers and kids across the country? We actually don’t know what’s going on with flu deaths in children across the country. This is highly unusual because every year the Public Health Agency of Canada collects this information and published it weekly, as part of the Public Health Agency of Canada’s flu watch program. This is the first year in decades that that data has not been made available during the respiratory virus season. We discovered after a lot of reporting on this that the Public Health Agency of Canada switched service providers on who is collecting that data. For whatever reason, that data has not been made available. So this is a huge black hole that can really compromise the ability of clinicians and health policy experts from mounting a response in real time or giving a warning signal to the rest of the country as to what might be coming their way. What kind of impact are all of these illnesses having on our public health care system? It’s been a very challenging few years for health care in Canada, and the hospitals are struggling across the country. You add in a respiratory virus season and there are patients who are in hallways, elective procedures are being cancelled or postponed, children are waiting unacceptable amounts of time. It’s a very difficult period right now in health care. Should we be paying attention to new COVID-19 variants these days? The sub variants remain vitally important. JN1, which is a sub variant of Omicron, is kind of similar in a sense to Omicron, in that it is infecting a lot of people and has quickly – within a matter of weeks – become the dominant COVID-19 variant spreading in Canada. There are researchers and clinicians who are studying variants all the time and it’s vital that they do so because we need to continue to understand where this virus is heading, how it’s changing. So far, there’s nothing to suggest that we’re in a much different, more severe place with JN1. It just continues to be something that we need to respond to and probably should be taking more protective actions against in just in terms of getting vaccinated and staying home when sick. How accurate are rapid tests in detecting these new strains of COVID-19? There’s a number of clinicians and experts who have seen – and a lot of us anecdotally have seen – that the test effectiveness seems to have gone down. Experts say they’re likely not as sensitive any more, because the variants that are in circulation are looking a lot different than the variants that the tests were designed to look for. At the same time, there was a recent report out from Global News suggesting that the company producing the tests actually edited some of the results to make the tests look more sensitive than they were. But if you have those respiratory virus symptoms, and you think you have COVID-19, and you test negative, test again. If those symptoms persist, just act as though you do have COVID-19 or another contagious virus. You don’t want to be heading out to a large family gathering if you have the flu, or COVID-19. How well are the COVID-19 vaccines matched to the variants that are in circulation now? The vaccines that are currently available are actually a pretty good match for the sub variant that is in circulation. The latest vaccine approved by Health Canada was designed to protect against a sub variant that was in circulation in early 2023. Now there’s a new sub variant on the scene – JN1 for instance. But all of these variants are sub variants of Omicron. They’re close enough relatives that you’re going to get good enough protection from them. It may not be 100 per cent, you may still even get some symptoms if you’re infected with COVID-19. But you’re not going to get severely ill, there’s less chance of spreading it, there’s less chance of severe outcomes, which is better, especially for those individuals who are at heightened risk of severe outcomes. Are people still getting vaccinated? The most current data from the federal government suggests that only around 15 per cent of the population received a booster this fall. So essentially, the vast majority of the population has little protection against the COVID-19 sub variants that are in circulation. So when you hear a lot of people saying they’re infected with COVID-19, that’s likely one of the reasons why. There’s a very contagious sub variant out there. And almost no one has been vaccinated against it. Public confidence in booster shots started to decline. Part of that is vaccine fatigue, COVID-19 fatigue. Part of it is also maybe lack of access, there’s not as many mass vaccination clinics. Part of it is also that lack of confidence. There’s so much information out there now, on questioning the vaccine. You’ve seen, legitimate health authorities in places like the United States actually saying it doesn’t work. How effective is the flu shot? Are people getting it? The flu shot has been available every year, and every year the vaccination numbers are pretty low. We don’t have numbers for across the country yet. If you look at Alberta, a place that does give out a lot of data, the numbers there are quite low. Overall, less than one in four people have been vaccinated. It’s the older age groups (60 plus) that have the highest vaccination rates. People in the younger age categories, even at risk children, the vaccination numbers are very low, even in the single digits. Some years the flu shot is not as good a match, this year is actually a really good match. The dominant strain of the flu going around is H1N1, and one of the strains that this year’s flu shot protects against is H1N1. So if you’re going to get vaccinated for the flu, this is a great year to do so because we know that there’s a really good match there. This interview was taken from a transcript of The Decibel podcast, and has been edited and condensed for clarity. These vaccines do work. And I think there’s a there’s a challenge here that we need to answer with lack of confidence.
By Munir Dharamshi
•
20 Jun, 2023
Welcome to our comprehensive patient handout on “Calcium – Dietary Sources and Drug Interactions.” This valuable tool has been specifically designed to assist pharmacists in patient consultations. As pharmacists, you play a crucial role in patient education, and this handout will supplement your patient counselling with information to help guide your patients on the use of milk and dairy products to meet their nutritional needs, while also addressing potential interactions with medications. Within this resource, your patients will find: Recommendations on the daily intake amount of calcium based on their age. Examples of calcium content in common milk and dairy products to help them reach their calcium needs through dietary intake. Common drug interactions with milk and/or dairy products to inform them on appropriate timing and spacing between medication administration and the consumption of milk and dairy products. Remember, this resource serves as a starting point to facilitate your patient consultations. It is essential to combine this information with your professional expertise and personalized guidance. Empower your patients with the knowledge they need to make informed decisions about their nutrition and medication management. More - https://opatoday.com/calcium-dietary-sources-and-drug-interactions
CONTACT
Telephone
(416) 750-4691
INFO@REMEDYSPHARMACY.CA
ADDRESS
Remedy's Lawrence Pharmacy
2683 Lawrence Avenue East
Unit 5 Ground Floor Pharmacy Entrance
Scarborough, ON. M1P 2S2
Tel: (416) 750-4691
Fax: (416) 750-2113
Cell: (647) 300-4691
http://www.torontotravelclinic.ca
http://www.torontotravelclinic.ca
CLINIC HOURS
- Mon - Fri
- -
- Saturday
- -
- Sunday
- Closed